Healthcare
How Artificial Intelligence is Transforming Clinical Trial Recruitment
How AI is Transforming Clinical Trial Recruitment
The medical world is shifting underneath our feet.
To keep up with the rising demands of empowered patients, physicians and pharma businesses regularly test innovative treatments and medicines during rigorous clinical trials.
But one misguided move can trigger a domino effect, such as when the wrong patients are selected for a clinical trial.
Today’s infographic comes to us from Publicis Health, and it highlights why the current model of clinical trial recruitment urgently needs to change.
The Cost of Clinical Trials
Clinical trials help to determine if a new treatment, drug, or device is safe for the larger patient population.
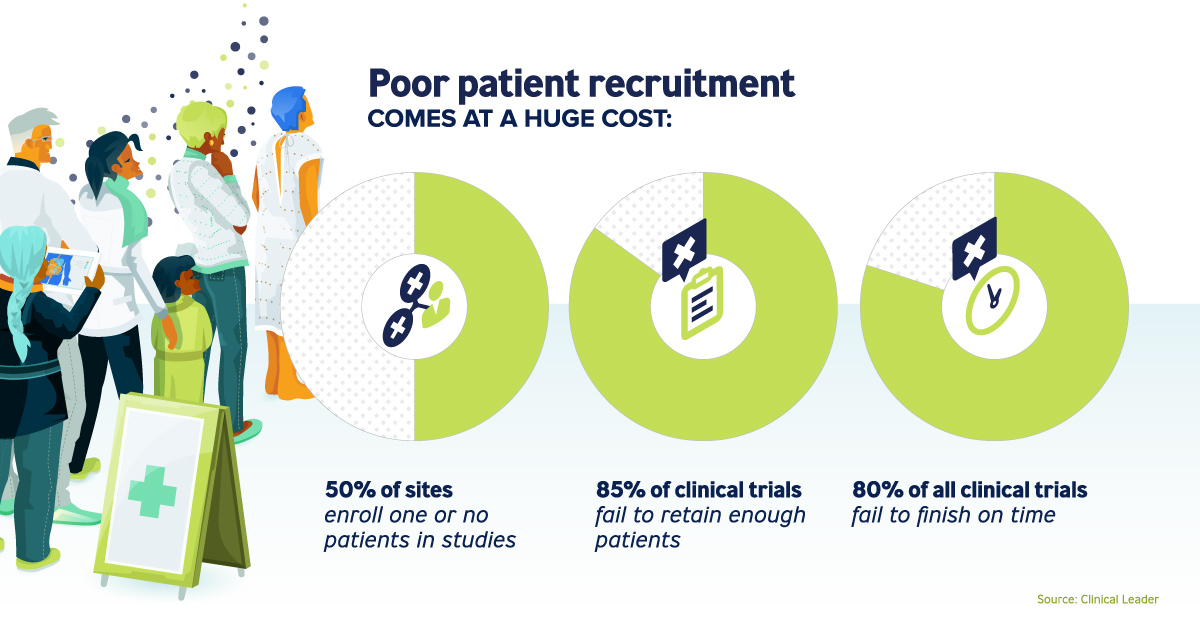
Patients are at the heart of these clinical trials, and poor patient recruitment has dire consequences:
- 50% of sites enroll one or no patients in studies
- 85% of clinical trials fail to retain enough patients
- 80% of all clinical trials fail to finish on time
A single trial can cost anywhere from $44 million to $115 million. But here’s the kicker – according to a CenterWatch survey, delays can cost a trial between $600,000 and $8 million per day.
For these reasons, it’s crucial for pharma trial sponsors to find the right fit for clinical trials from the start.
A 360° View
The healthcare industry is moving towards a people-based marketing approach, to discover and engage the right patient one-on-one.
Advanced technology and connected patient data work in tandem with millions of real-time consumer behaviors, creating a rich and accurate profile of the perfect patient match.
The use of artificial intelligence, machine learning, and predictive analytics unearth further insights, weighting those patients with the behavioral tendencies most suited for the trial:
Omni-channel targeting
Actively reaching out to patients, wherever they are.
Predictive analytics
Continually refining media channels and messaging to further patient interest.
Ongoing communications
Nurturing relationships with patients, starting with the initial outreach.
Transforming Value
Applying a people-based approach to patient recruitment has a myriad of benefits, many of which live on long after the original trial’s completion.
| Advantage | Value added | |
|---|---|---|
| Recruitment | - Accurate insight generation - Real time optimization - Faster and improved quality | - More efficient - Increased conversion - Reduced costs |
| Engagement | - Behavioral-based messaging - Personalized trial participation experiences | - Precise engagement at scale - Drives patient adherence and retention during a trial |
| Long-term benefits of data collected | - Develops patient profiles for future trials - Guides the planning of the patient demographic - Informs drug launch activities | - Accelerates recruitment and reduces start-up costs - Speeds up commercialization of new drugs - Supports disease awareness and educational campaigns |
As clinical trials are successfully completed on time – allowing new drugs to reach the market faster than before – patients will benefit from easier access to groundbreaking treatments.
This is part five of a seven part series. Stay tuned by subscribing to Visual Capitalist for free, as we wrap up with the final two transformative forces shaping the future of healthcare.
Healthcare
The Cost of an EpiPen in Major Markets
This visualization compares EpiPen prices around the world, with the U.S. having the highest prices by far.

The Cost of an EpiPen in Major Markets
This was originally posted on our Voronoi app. Download the app for free on iOS or Android and discover incredible data-driven charts from a variety of trusted sources.
EpiPens are auto-injectors containing epinephrine, a drug that can treat or reverse severe allergic reactions, potentially preventing death.
The global epinephrine market was valued at $1.75 billion in 2022 and is projected to reach $4.08 billion by 2030. North America represents over 60% of the market.
EpiPens, however, can be prohibitively expensive in some regions.
In this graphic, we present estimated EpiPen prices in major global markets, compiled by World Population Review and converted to U.S. dollars as of August 2023.
Why are U.S. Prices so High?
The U.S. stands out as the most expensive market for EpiPens, despite over 1 million Americans having epinephrine prescriptions. After Mylan (now part of Pfizer) acquired the rights to produce EpiPens in the U.S. in 2007, the cost of a two-pack skyrocketed to $600, up from about $60.
| Country | Price (USD) |
|---|---|
| 🇺🇸 U.S. | 300* |
| 🇯🇵 Japan | 98 |
| 🇩🇪 Germany | 85 |
| 🇨🇦 Canada | 80 |
| 🇫🇷 France | 76 |
| 🇦🇺 Australia | 66 |
| 🇬🇧 UK | 61 |
| 🇮🇳 India | 30 |
*Per unit cost. Commonly sold as a two-pack, meaning total cost is equal to $600
Former Mylan CEO Heather Bresch defended the price hikes to Congress, citing minimal profit margins. Mylan eventually settled with the U.S. government for a nine-figure sum.
Notably, EpiPens are available at a fraction of the cost in other developed countries like Japan, Germany, and Canada.
Making EpiPens More Affordable
Efforts to improve EpiPen affordability are underway in several U.S. states. For instance, the Colorado House approved a $60 price cap on epinephrine, now under review by the state Senate.
Similar measures in Rhode Island, Delaware, Missouri, and Vermont aim to ensure insurance coverage for epinephrine, which is not currently mandatory, although most health plans cover it.
-

 Mining1 week ago
Mining1 week agoGold vs. S&P 500: Which Has Grown More Over Five Years?
-

 Markets2 weeks ago
Markets2 weeks agoRanked: The Most Valuable Housing Markets in America
-

 Money2 weeks ago
Money2 weeks agoWhich States Have the Highest Minimum Wage in America?
-

 AI2 weeks ago
AI2 weeks agoRanked: Semiconductor Companies by Industry Revenue Share
-

 Markets2 weeks ago
Markets2 weeks agoRanked: The World’s Top Flight Routes, by Revenue
-
 Countries2 weeks ago
Countries2 weeks agoPopulation Projections: The World’s 6 Largest Countries in 2075
-
 Markets2 weeks ago
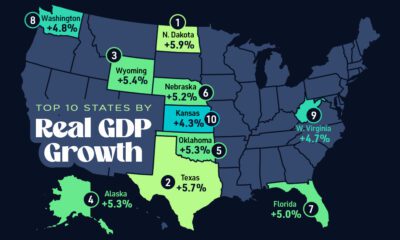
Markets2 weeks agoThe Top 10 States by Real GDP Growth in 2023
-

 Demographics2 weeks ago
Demographics2 weeks agoThe Smallest Gender Wage Gaps in OECD Countries